The High Cost of Cognitive Load
How Cognitive Load Theory can reshape how we understand decision-making in high-stakes environments.
Human Errors And Cognitive Load

In any system, the human mind is the most likely source of error. It is fallible, error-prone, imperfect, yet wondrous. It’s the tool that has incited all of human innovation— while equally serving as the instrument of immense destruction. Although modern research recognizes the mind’s many capabilities, uncovering the mechanisms behind its operation has been a central objective for philosophers, psychologists, and neuroscientists since the earliest days of human inquiry. The psychology and human factors fields have made great strides in uncovering the link between human behavior and thought processes in relation to the environment in which they inhabit. One recent unearthing is called Cognitive Load Theory (CLT), proposed by the Australian psychologist John Sweller in 1988. Cognitive Load Theory describes the process of information perception, encoding, and storage. This theory helps to explain why certain human behaviors may occur in different environments due to cognitive load— that is the mental effort needed to complete a task. This theory is applicable to almost any field in industries or occupations— what Georgetown University computer science professor and author Cal Newport refers to as knowledge work and non-knowledge work— but its implications are profound in the healthcare industry. In the field of healthcare, decision-making is at the highest stakes possible and involves operators in academic, clinical, and occupational roles. Poor decision-making in healthcare can have grave consequences on the system users.
Accidents in healthcare are not uncommon. As the Australian pilot and human factors professor Sidney Dekker reports, “The first national study in Canada on adverse events in acute care hospitals found that in 2000, of 2.5 million adult hospital admissions, 7.5% (185,000) resulted in an adverse event. Of these, 37% (70,000) were considered preventable,” (Dekker, 2011). A seemingly minor error— whether in surgery, medication admin- istration, or diagnostics— can result in irreversible damage or even death to a patient. Therefore, understanding what cognitive load theory entails and how to apply it is critical in the high-impact field of healthcare. Leveraging its key tenets offers the potential to mitigate preventable errors, enable more cogent decision-making, and ultimately facilitate a more effective and safer healthcare system.
What is Cognitive Load Theory?

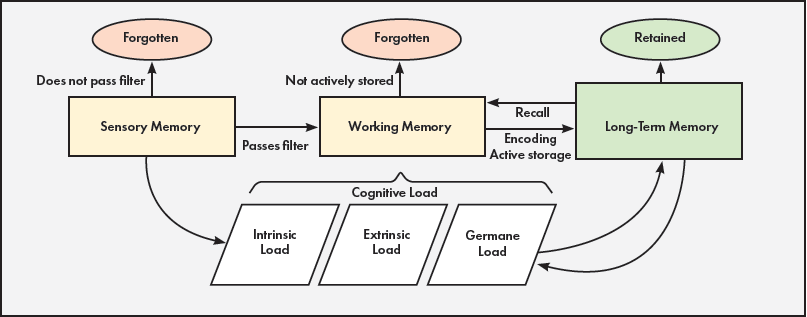
Dr. John Sweller's Cognitive Load Theory can be broken down into three types: intrinsic, extraneous, and germane. Intrinsic cognitive load is “the inherent difficulty of the subject matter” and “indigenous to the to-be-learned information and task” (“Cognitive Load Theory”). Intrinsic load is like opening a complex CAD model or a graphics-intensive video game on a computer. It naturally demands more random access memory (RAM). The more complex or intensive a task is, the more cognitive resources it will require. Extraneous load includes the "cognitive processes that are irrelevant for successful comprehension and learning,” (“Cognitive Load Theory”). Extraneous load includes "unnecessary information or activities, such as noise or nongermane activity or stimuli” (“Cognitive Load Theory”). Extraneous load can be analogized to a computer needing to run Excel while having Spotify, multiple Chrome tabs, and other useless applications running in the background. All of the non-essential tasks will eat into the computer's RAM usage and cause Excel to run more poorly. Extraneous load can hinder a person’s performance on a specific task. The final type of cognitive load is Germane. Germane cognitive load assists “the learner to construct viable and relevant schemata,” (“Cognitive Load Theory”). Germane load “is the necessary and desirable cognitive load for comprehension and learning,” (“Cognitive Load Theory”). Germane load refers to the mental effort the brain uses to understand, learn, and internalize information. It is similar to the process of a computer saving a file. First, the data is handled by the computer's RAM (working memory) before being stored more permanently on the solid state drive (SSD). In the human mind, germane load represents the cognitive work involved in transferring information from working memory to long-term memory by building meaningful connections though schemas.
Figure 1. Key areas of cognitive load theory.
Cognitive Load in the Healthcare Industry

Healthcare practitioners operate in highly complex environments with the looming possibility of immense consequences. Every decision a healthcare professional makes has the potential to adversely impact the system users (patients). Examining each of the three primary pillars of cognitive load theory can help individuals better understand the challenges of the healthcare sector and reveal paths to mitigate these errors, ultimately creating an experience more efficient and effective to its users.
Intrinsic load regards the innate complexity of medical care, knowledge, and procedures. A successful emergency room physician must be able to quickly interpret vital signs, perform timely tasks based on deep-rooted knowledge, and follow medical procedures. As described by the Agency for Healthcare Research and Quality, intrinsic load is the, "effort required to learn a new task, process relevant clinical information, or perform procedural steps” ("Cognitive Load Theory and Its Impact on Diagnostic Accuracy"). Extraneous cognitive load is perhaps one of the most notable in the healthcare field. Extraneous load refers to everything non-essential that the operator must cognitively process; it is the interference in the way of achieving the optimal task. Clinical environments are home to constant alarms, beeps, and alerts. Many of these do not require immediate attention, though they still go off, becoming unnecessary stimuli. It draws from the attention of healthcare workers and can hinder the performance of other more essential tasks. This is also referred to as “alarm fatigue.” Extraneous load can include “information presented in an ineffectual way (e.g., overly complicated electronic record visuals),” or even “load from the external environment (e.g., chaotic surrounding environment) or load from the internal environment (e.g., stress from a recent negative patient interaction),” ("Cognitive Load Theory and Its Impact on Diagnostic Accuracy"). The final pillar is germane load, which can be represented by physicians who have more experience and have built robust schemas of various situations that occur in the working environment. A well-seasoned practitioner may not just have an extensive memory, but that person might be able to make better decisions than a non-experienced individual when presented with a situation and an array of information at his or her disposal. For instance, a healthcare professional may, “use germane cognitive load to pull in congestive heart failure diagnostic schemas to compare this patient’s clinical presentation with their typical representation of a patient with heart failure” ("Cognitive Load Theory and Its Impact on Diagnostic Accuracy").
The Perils of Multitasking in Healthcare

Healthcare practitioners, especially nurses, are expected to multitask throughout the workday. Multitasking involves rapidly switching between various tasks or completing two or more tasks concurrently. Shifting between two activities, also known as context switching, is linked to degraded job performance, additional stress, and a decrease in performance. “Information workers perform jobs that demand constant multitasking, leading to context switches, productivity loss, stress, and unhappiness. Systems that can mediate task transitions and breaks have the potential to keep people both productive and happy,” (Serebrenik et al., 2020). Any time a worker needs to change tasks, he or she will need to draw upon cognitive resources to attend to the new task while still keeping some memory of the old task. “A lot of things happen then {when you engage in context-switching}: we need to allocate attention to our task at hand, but then suddenly we attend to the interruption, trying to keep track of the interrupted tasks in our minds, all while resisting new distractions. When we do all this under time pressure and for an extended period, the overtaxed governor of your mind struggles to keep you on your goals. That's when you start to see an impact on performance,” (Mark, 2023). As Gloria Mark of the University of California, Irvine, points out, this process can greatly hinder one’s performance. A degradation in performance can be disastrous in the healthcare industry. Tending to too many tasks at once can jeopardize the safety and well-being of patients. “Multi-tasking typically results in increased time to task completion, increased stress, possible memory lapses and subsequent errors and accidents,” (Douglas et al., 2017). Researchers have conducted tests in different work environments, but the results are still notable. “Results show that developers who work on 2 or 3 projects spend on average 17% of their effort on context switching between tasks from different projects. Developers who were involved in more projects tend to have more cross-project work interruptions,” (Tregubov et al., 2017). Simply put, the context switching portion of multitasking is cognitively intense. “It {multitasking} also increases the difficulty participants experience in redirecting attention from a previously relevant stimulus to a currently relevant one,” (Douglas et al., 2017). Multitasking degrades performance, increases the time to complete tasks, draws upon precious cognitive resources, and opens areas for error.
While multitasking is generally viewed in a negative light in the community of academia and research, nurses are expected to manage multiple different tasks simultaneously. “In a study examining over 1000 h of observational data of doctors and nurses in teaching hospitals, the rates at which clinicians performed two tasks in parallel ranged from 9.2 multitasking events per hour in an emergency department, to 17.3 on hospital wards,” (Douglas et al., 2017). Considering multitasking degrades perfor- mance and opens up regions of error, this can be detrimental to patients and the healthcare industry. “Error rates increased significantly if physicians were interrupted or multitasked while prescribing,” (Westbrook, Johanna I, et al., 2018). This can be especially negative when healthcare workers are prescribing medications that must be delivered in precise dosages. “Multitasking during prescribing was significantly associated with an increased rate of legal/procedural errors ,” (Westbrook, Johanna I, et al., 2018). Multitasking can be the catalyst for errors. There are two main types of multitasking events that can ultimately lead to different errors and outcomes.
First, there is concurrent multitasking, also referred to as dual-task interference or dual- tasking. Dual-tasking is the action of completing two or more tasks at once. An example would be a nurse asking a patient questions about his or her medical history while preparing an intravenous syringe. The second is interleaved multitasking. Interleaved multitasking describes "switching between tasks that are progressing in parallel," (Douglas et al., 2017). Perhaps a nurse is administering an IV solution to patient A. If an alarm goes off at patient B’s bed, and he or she leaves to attend to the alarm and then returns to A, that individual would have just performed interleaved multitasking.
Concurrent multitasking “carries a performance cost in terms of decreased accuracy, and increased reaction time to environmental stimuli," (Douglas et al., 2017). Past research has demonstrated that operator reaction times of the task that was presented after the primary one suffered diminished performance. “This effect has also been demonstrated in driver simulator studies of braking in response to brake lights from a leading vehicle, even when participants are instructed to give priority to the braking response," (Douglas et al., 2017). While driving is certainly different from healthcare, this research is nevertheless applicable. “Driving while using a phone can be thought of as concurrent multitasking with two tasks in different modalities (i.e. the driving task is visual-manual, while the phone task is auditory),” (Douglas et al., 2017). Concurrent multitasking is common in both environments (especially across modalities— referring back to the alarm fatigue phenomenon discussed on page 4) and any activity requires undivided attention for optimal performance.
In a different study focusing on driving performance with the use of smartphone digital assistants (SDAs) like Siri, performance was affected even after the concurrent multitasking event ended. “The delays in returning to baseline driving performance after completing a secondary task raise concerns about the usage of in-vehicle devices while driving as the effects of the delays last beyond the cessation of the Smartphone Digital Assistant (SDA) interaction,” (Turrill et al., 2016). In other words, driving performance was reduced even after the concurrent multitasking event of driving and communicating with the SDA was over. This demonstrates that there is a residual cost after the operator switches back to the primary task. “Upon dual-task cessation, the participants’ performance did not immediately return to baseline levels. Thus, just because a driver has terminated a call or completed a voice-dictated text does not mean that they are no longer impaired,” (Turrill et al., 2016). More interestingly, a driver using a smartphone can experience comparable task performance to someone under the influence of alcohol. “Drivers using a cell phone exhibited a delay in their response to events in the driving scenario and were more likely to be involved in a traffic accident. Drivers in the alcohol condition exhibited a more aggressive driving style, following closer to the vehicle immediately in front of them, necessitating braking with greater force. With respect to traffic safety, the data suggest that the impairments associated with cell phone drivers may be as great as those commonly observed with intoxicated drivers,” (Strayer et al., 2006). Concurrent multitasking can result in worsened performance, and its effects will still linger afterwards.
Interleaved multitasking has similar effects to concurrent in regards to task performance. “When an individual switches tasks, they have to ‘reconfigure’, or activate a new task set. This is called task set reconfiguration, and it results in an increased response time to the new task, and an increased likelihood of errors," (Douglas et al., 2017). Not only is the response time increased, but the likelihood of errors also increases. Interleaved multitasking simply makes the working experience more difficult and cognitively intensive. Like concurrent multitasking there is, “a residual cost associated with interleaved multi-tasking occurs regardless of the amount of time available to participants to prepare for the switch,” (Douglas et al., 2017). Specifically in the Australian healthcare system, there has been research into the effects of interleaved multitasking. “For example, Australian nurses at two hospitals were found to make significantly more medication administration errors and more severe errors as interruptions increased. However, it is also important to recognise that not all interruptions are negative and some may in fact be life-saving in a clinical setting. Training and specific interventions may reduce potential negative impacts of interruptions. Multitasking has also been shown in other environments to increase the risk of error,” (Li et al., 2024). It’s vital to note that at times a secondary task can far outweigh the original task. For instance, if patient B has a heart attack, then a nurse should cease observing patient A’s vitals to attend to patient B’s more urgent situation. When the next situation is less pressing, the increased errors and reduction in performance must be considered. Nevertheless, there isn’t a copious amount of research into multitasking in the clinical setting. As Macquarie University senior research fellow Ling Li pointed out, "We still know very little about the effects of multitasking on clinical work and, given the high rates observed, we have identified it as an area warranting further investigation," (Li et al., 2024).
Decision-Making in Healthcare

Medical professionals are often tasked with making difficult and timely decisions on a daily basis. From deciding what medications to prescribe or reading and analyzing Magnetic Resonance Imaging (MRI) scans, patients’ outcomes can reside in the cognitive processes of the professionals caring for them. “Medical decisions are vital, to both patients and society. They are difficult, and may provide positive outcomes, or poor complications. They test doctors maximally, and provide insight into the effectiveness of doctors,” (Masic, 2022). Decision-making among professionals is a pivotal area of the healthcare sector.
Within a complex work environment like a hospital, making decisions can become more difficult. This is due to the frequent multitasking and the inherent chaos of the environment. “In addition, an Emergency Department (ED) is an example of a multifaceted organization composed of complex social environments, where interruptions are frequent and disruptive. Such environments, where decisions are made under time pressure and with incomplete information, have been considered conducive to error,” (Laxmisan et al. 2007). A dynamic environment with frequent disruptive interruptions poses as a breeding ground for errors that could stem in the decision-making process. “This process of decision-making in the emergency department is made more complex by the large number of patients under the care of a single clinician at any one point in time as well as the number of distributed tasks across personnel, information systems and laboratories,” (Laxmisan et al. 2007).
Fatigue can also affect a practitioner’s ability to make decisions. "Individuals with mental fatigue may have lower risk tolerance and consequently be risk averse. Our research contributes to the understanding of the effects of fatigue on decision-making by showing that mental fatigue affects both the risk preferences and the processing of feedback," (Jia, Lin, and Wang). Huiqiao Jia of the National Taiwan University of Science and Technology and team conducted a gambling task in which fatigued and non-fatigued students were tasked with making a risky or non-risky decision. It found that the fatigued group tended to make conservative choices. “Therefore, it appeared that mental fatigue had an impact on the risk preference of the individuals when making risk decisions. The mean ratio of risk preference in the fatigue group was 0.44, while it was 0.50 in the non-fatigue group, indicating that the participants with mental fatigue tended to make more conservative choices than participants with no fatigue in their risk choices," (Jia, Lin, and Wang).
Managing Cognitive Load in Healthcare

The goal in any system is not to eliminate cognitive load. Rather, the goal is to reduce extraneous load, manage and break down intrinsic load, and enhance germane learning. “Effective countermeasures do not start with individual human beings who themselves were at the receiving end of much prior trouble,” (Dekker, 2011). Therefore, healthcare administrators must work to ensure the work environment facilitates an environment conducive to the three core tenets of cognitive load theory.
Perhaps the most notable aspect of CLT to engage with is reducing extraneous load. There are many venues in which hospital managers can reduce extraneous load. Hospitals are notorious for recurring alarms and alerts that in some cases are irrelevant to tasks in which the medical staff are working on. The influx of alarms can be cognitively exhausting to deal with, creating ‘alarm fatigue.’ “Alarm fatigue is sensory overload when clinicians are exposed to an excessive number of alarms, which can result in desensitization to alarms and missed alarms,” (Sendelbach and Funk, 2013). The medical staff’s exposure to constant alarms—with 72 to 99 percent being false— can have negative impacts on patients (Sendelbach and Funk, 2013). “As new devices are introduced, the number of alarms to which a healthcare professional may be exposed may be as high as 1000 alarms per shift. The US Food and Drug Administration has reported over 500 alarm-related patient deaths in five years,” (Ruskin and Hueske-Kraus, 2015).
Two ways to reduce extraneous load is by mitigating unnecessary information and altering the method in which data is presented. Regarding the information itself, there are generally three types, “(1) technically false alarms where the cause of the alarm does not correspond to reality, (2) technically correct but clinically irrelevant (i.e. non-actionable) alarms where the cause of the alarm is rooted in reality but there is no consequence to the alarm, and (3) technically correct and clinically relevant (i.e. actionable) alarms,” (Schmid et al. and Chromik et al., 2011). Mitigating technically false alarms and technically correct but clinically irrelevant items is key to reducing alarm fatigue. By ensuring that clinicians and nurses are only alerted to consequential, time-sensitive information, alarm systems can better enable decision-making rather than hinder it. The result is a more cognitively endurable environment where alarms regain their intended purpose. The purpose is to signal an urgent, high-priority event, not deliver unnecessary or inaccurate information that just increases one's cognitive extraneous load.
Elham Asgari of Michigan Technological University suggests that the way data is presented plays a massive role in cognitive load as well. The routes in which large data sets are provided can become cognitively overwhelming to users, contributing to burnout (Asgari et al., 2024). “Several factors, such as the presentation of information in the Electronic Health Record (EHR), the specialty, the health care setting, and the time spent completing documentation and navigating systems, can contribute to this excess cognitive load and result in burnout,” (Asgari et al., 2024). Especially regarding EHRs, there are many ways to alter the way in which the data is presented. “Potential strategies to mitigate this might include improving user interfaces, streamlining information, and reducing documentation burden requirements for clinicians. New technologies may facilitate these strategies,” (Asgari et al., 2024). Some methods include reducing the time spent on navigating the software, pinpointing large data sets to only the vital information, improving the user interfaces to focus on simplicity, and incorporating effective methods of data visualization (Asgari et al., 2024). Still, at the core of these updated ways to deliver and present information is CLT. “Using cognitive science to navigate information overload to decrease frustration while increasing performance can impact patient outcomes and provider experience. Understanding cognitive science when designing information presentation systems is critical to future health care delivery as complexity increases,” (Harry et al.).
Education for Cognitive Load Theory
Incorporating CLT in healthcare begins with education. Marco Mancinetti, an attending physician at the university of Fribourg, proposes to have education tailored to Cognitive Load Theory for medical professionals. “We have indicated that the CLT offers interesting perspectives on how to improve learning and help redesign clinical teaching. Its aim is to facilitate the germane cognitive load, which results from the optimization of the intrinsic load while also minimizing the extrinsic cognitive load. The teacher should adapt the education design and pitch this accordingly to the level of the learners, in order to enable them to build new knowledge based on their actual level of expertise,” (Mancinetti et al., 2019).
Mancinetti suggests methods to improve the cognition of medical professionals across all aspects of the healthcare field. To manage intrinsic load, Mancinetti recommends to focus on the critical elements of a data set first and to gradually increase the complex- ity. For extraneous cognitive load, he recommends to provide worked examples of problems to students, utilize different modalities such as visual displays along with text, and avoid notifications from external sources when working with patients, among others. “Clinicians frequently receive notification of the identical information via a page, a separate call from the lab, a flag in the lab page and an email. These well-intentioned notifications create a noise making it difficult to process other data. For the clinical teacher, it is essential to recognize this and to point out the essentials,” (Mancinetti et al., 2019). Finally, he recommends ways to bolster the germane cognitive load. This includes approaching tasks from different perspectives, allowing the learners to explain procedures without just referring to a textbook, and asking them for their rationale when a decision was made. This goes hand-in-hand with critical thinking abilities, a skill necessary to a safe and effective healthcare industry. “As a clinical teacher you prompt the resident to give the rationale behind a medication choice. The resident should be able to explain the risks or benefits of such medication by pondering side effects and the expected effects of the treatment in the specific clinical situation,” (Mancinetti et al., 2019).
Creating an environment aligned with the principles of Cognitive Load Theory has the potential to reduce medical errors, enhance decision-making abilities, and ease the cognitive burden on healthcare pro- fessionals, who are already stretched far and thin. “When the working memory of the learner is overloaded, learning is hindered and the resulting clinical performance is impaired. This can cause errors and eventually harm patients,” (Mancinetti et al., 2019). To facilitate this ideal vision, education is the logical first step.
Understanding the System Operator
Improving the quality of healthcare starts with understanding the users themselves. No system will ever be perfect, but there is considerable room for improvement within the United States’ healthcare industry. “Experts estimate that as many as 98,000 people die in any given year from medical errors that occur in hospitals,” (Kohn et al., 2011). Many of these deaths are attributed to human error, according to the textbook To Err is Human. “To Err Is Human asserts that the problem is not bad people in healthcare– it is that good people are working in bad systems that need to be made safer,” (Kohn et al., 2011). These errors primarily stem from a flawed system and the environment in which healthcare professionals operate.
Implementing Cognitive Load Theory into the healthcare sector is about reengineering environments to facilitate better decision- making, mitigate human errors, and cultivate a population of highly-skilled healthcare professionals. Doing so will not only benefit system providers, but improve patient outcomes and cultivate a more sustainable future for those dedicating their lives to caring for others.
Works Cited
Asan, Onur, Paul Smith, and Enid Montague. “More Screen Time, Less Face Time—Implications for EHR Design.” Journal of Evaluation in Clinical Practice, vol. 20, no. 6, 2014, pp. 896–901. https://doi.org/10.1111/jep.12182.
Asgari, Elham, et al. “Impact of Electronic Health Record Use on Cognitive Load and Burnout Among Clinicians: Narrative Review.” JMIR Medical Informatics, vol. 12, 2024, article no. e55499, https://doi.org/10.2196/55499.
“Cognitive Load Theory.” ScienceDirect Topics, Elsevier, https://www.sciencedirect.com/topics/psychology/cognitive-load-theory. Accessed 18 Apr. 2025.
"Cognitive Load Theory and Its Impact on Diagnostic Accuracy." Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services, https://www.ahrq.gov/sites/default/files/wysiwyg/diagnostic/resources/issue-briefs/dxsafety-cognitive-load-theory.pdf. Accessed 18 Apr. 2025.
Chromik, Jonas, et al. “Computational Approaches to Alleviate Alarm Fatigue in Intensive Care Medicine: A Systematic Literature Review.” Frontiers in Digital Health, vol. 4, 16 Aug. 2022, article no. 843747. https://doi.org/10.3389/fdgth.2022.843747.
Dekker, Sidney. Patient Safety: A Human Factors Approach. CRC Press, 2011. Chapter 2, pp. 33–54.
Douglas, Heather E., et al. “Improving Our Understanding of Multi-Tasking in Healthcare: Drawing Together the Cognitive Psychology and Healthcare Literature.” Applied Ergonomics, vol. 59, 2017, pp. 45–55. Elsevier, https://doi.org/10.1016/j.apergo.2016.08.021.
Gandhi, Tejal K., et al. “How Can Artificial Intelligence Decrease Cognitive and Work Burden for Front Line Practitioners?” JAMIA Open, vol. 6, no. 3, 2023, ooac079. https://doi.org/10.1093/jamiaopen/ooad079.
Harry, Elizabeth M., et al. “Using Cognitive Load Theory to Improve Posthospitalization Follow-Up Visits.” Applied Clinical Informatics, vol. 10, no. 4, 21 Aug. 2019, pp. 610–614. https://doi.org/10.1055/s-0039-1694748.
Howard, Steven K. “Sleep Deprivation and Physician Performance: Why Should I Care?” Baylor University Medical Center Proceedings, vol. 18, no. 2, 2005, pp. 108–112. Taylor & Francis, https://doi.org/10.1080/08998280.2005.11928045.
Institute of Medicine (US) Committee on Quality of Health Care in America. To Err Is Human: Building a Safer Health System. National Academies Press, 2000. https://doi.org/10.17226/9728.
Jia, Huiqiao, Chiuhsiang Joe Lin, and Eric Min-yang Wang. “Effects of Mental Fatigue on Risk Preference and Feedback Processing in Risk Decision-Making.” Scientific Reports, vol. 12, 2022, article no. 10695, https://doi.org/10.1038/s41598-022-14682-0.
Landrigan, Christopher P., et al. “Effect of Reducing Interns' Work Hours on Serious Medical Errors in Intensive Care Units.” The New England Journal of Medicine, vol. 351, no. 18, 2004, pp. 1838–1848, https://doi.org/10.1056/NEJMoa041406.
Laxmisan, Archana, et al. “The Multitasking Clinician: Decision-Making and Cognitive Demand during and after Team Handoffs in Emergency Care.” International Journal of Medical Informatics, vol. 76, issues 11–12, Nov.–Dec. 2007, pp. 801–811. Elsevier, https://doi.org/10.1016/j.ijmedinf.2006.09.019.
Li, Ling, et al. “What Do ICU Doctors Do? A Multisite Time and Motion Study of the Clinical Work Patterns of Registrars.” Australian Critical Care, vol. 37, no. 1, 2024, pp. 18–26. Elsevier, https://doi.org/10.1016/S1441-2772(23)01483-7.
Mancinetti, Marco, Sissel Guttormsen, and Christoph Berendonk. “Cognitive Load in Internal Medicine: What Every Clinical Teacher Should Know about Cognitive Load Theory.” European Journal of Internal Medicine, vol. 60, 2019, pp. 4–8. Elsevier, https://dme.childrenshospital.org/wp-content/uploads/2019/06/Cognitive-load-in-internal-medicine-_What-every-clinical-teacher-should-know-about-cognitive-load-theory.pdf.
Mark, Gloria. Attention Span: A Groundbreaking Way to Restore Balance, Happiness and Productivity. Hanover Square Press, 2023.
Masic, 2022, Izet. “Medical Decision Making – An Overview.” Acta Informatica Medica, vol. 30, no. 3, 2022, pp. 230–235. https://doi.org/10.5455/aim.2022.30.230-235.
Pashler, Harold. “Dual-Task Interference in Simple Tasks: Data and Theory.” Psychological Bulletin, vol. 116, no. 2, 1994, pp. 220–244, https://doi.org/10.1037/0033-2909.116.2.220.
Ruskin, Keith J., and Dirk Hueske-Kraus. “Alarm Fatigue: Impacts on Patient Safety.” Current Opinion in Anesthesiology, vol. 28, no. 6, Dec. 2015, pp. 685–690. https://doi.org/10.1097/ACO.0000000000000260.
Schmid, Felix, et al. “The Wolf Is Crying in the Operating Room: Patient Monitor and Anesthesia Workstation Alarming Patterns During Cardiac Surgery.” Anesthesia & Analgesia, vol. 112, no. 1, Jan. 2011, pp. 78–83. https://doi.org/10.1213/ANE.0b013e3181fcc504.
Sendelbach, Sue, and Marjorie Funk. “Alarm Fatigue: A Patient Safety Concern.” AACN Advanced Critical Care, vol. 24, no. 4, 2013, pp. 378–386. https://doi.org/10.1097/NCI.0b013e3182a903f9.
Serebrenik, Alexander, et al. “Studying Interruptions and Task Switching in Software Development: A Replication Experiment.” Proceedings of the 2020 ACM/IEEE 42nd International Conference on Software Engineering: Software Engineering in Practice (ICSE-SEIP), 2020, pp. 187–196. Association for Computing Machinery, https://doi.org/10.1145/3313831.3376817.
Strayer, David L., Frank A. Drews, and Dennis J. Crouch. “A Comparison of the Cell Phone Driver and the Drunk Driver.” Human Factors: The Journal of the Human Factors and Ergonomics Society, vol. 48, no. 2, 2006, pp. 381–391. SAGE Publications, https://doi.org/10.1518/001872006777724471.
Taffinder, N.J., et al. “Effect of Sleep Deprivation on Surgeons' Dexterity on Laparoscopy Simulator.” The Lancet, vol. 352, no. 9135, 10 Oct. 1998, p. 1191, https://doi.org/10.1016/S0140-6736(05)79991-1.
Tregubov, Alexey, et al. "Impact of Task Switching and Work Interruptions on Software Development Processes." Proceedings of the 2017 International Conference on Software and System Process (ICSSP '17), 2017, pp. 132–136. Association for Computing Machinery, https://doi.org/10.1145/3084100.3084116.
Turrill, Jonna, et al. “The Residual Costs of Multitasking: Causing Trouble down the Road.” Proceedings of the Human Factors and Ergonomics Society Annual Meeting, vol. 60, no. 1, 2016, pp. 1967–1970. SAGE Publications, https://doi.org/10.1177/1541931213601448.
Venkat, Manu V., et al. “Using Cognitive Load Theory to Improve Teaching in the Clinical Workplace.” MedEdPORTAL, vol. 16, 2020, p. 10983. https://doi.org/10.15766/mep_2374-8265.10983.
Warner, B. W., et al. “Study of Surgical Resident Working Hours and Time Utilization.” Journal of Surgical Research, vol. 48, no. 6, June 1990, pp. 606–610. https://doi.org/10.1016/0022-4804(90)90239-x.
Westbrook, Johanna I, et al., 2018 “Task Errors by Emergency Physicians Are Associated with Interruptions, Multitasking, Fatigue and Working Memory Capacity: A Prospective, Direct Observation Study.” BMJ Quality & Safety, vol. 27, no. 8, 9 Jan. 2018, pp. 655–663, https://doi.org/10.1136/bmjqs-2017-007333.
Wood, Eileen, et al. “Examining the Impact of Off-Task Multi-Tasking with Technology on Real-Time Classroom Learning.” Computers & Education, vol. 58, no. 1, Jan. 2012, pp. 365–374. Elsevier, https://doi.org/10.1016/j.compedu.2011.08.029.